Telemedicine Appointments Are Now Available
Your Trusted Double - Board Certified Gastroenterologist




For More Information on this topic, visit:
Theories about what causes ulcerative colitis abound, but none have been proven. The most popular theory is that the body’s immune system reacts to a virus or a bacterium by causing ongoing inflammation in the intestinal wall.
People with ulcerative colitis have abnormalities of the immune system, but doctors do not know whether these abnormalities are a cause or a result of the disease. Ulcerative colitis is not caused by emotional distress or sensitivity to certain foods or food products, but these factors may trigger symptoms in some people.
A thorough physical exam and a series of tests may be required to diagnose ulcerative colitis.
Blood tests may be done to check for anemia and inflammatory markers, which could indicate bleeding in the colon or rectum. Blood tests may also uncover a high white blood cell count, which is a sign of inflammation somewhere in the body. By testing a stool sample, the doctor can detect bleeding or infection in the colon or rectum.
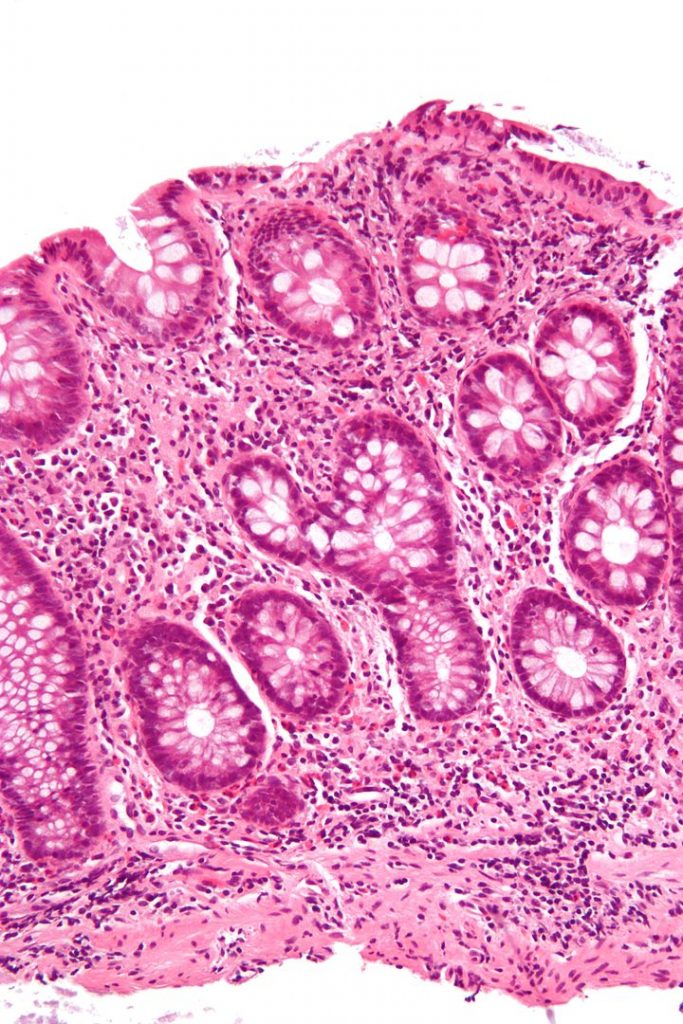
The doctor may do a colonoscopy or sigmoidoscopy. For either test, the doctor inserts an endoscope–a long, flexible, lighted tube connected to a computer and TV monitor–into the anus to see the inside of the colon and rectum. The doctor will be able to see any inflammation, bleeding, or ulcers on the colon wall. During the exam, the doctor may do a biopsy, which involves taking a sample of tissue from the lining of the colon to view with a microscope. A CT Scan of the abdomen and pelvis or rarely a barium enema x-ray of the colon may also be required. This is another method of visualizing the colon and is often used when pain is present.
Treatment for ulcerative colitis depends on the seriousness of the disease. Most people are treated with medication, and in the vast majority of patients, control of symptoms and remission are successful In severe cases, a patient may need surgery to remove the diseased colon. Surgery is the only complete cure for ulcerative colitis.
Some people whose symptoms are triggered by certain foods are able to control the symptoms by avoiding foods that upset their intestines, like highly seasoned foods, raw fruits and vegetables, or milk sugar (lactose). Each person may experience ulcerative colitis differently, so treatment is adjusted for each individual. Emotional and psychological support is important.
Some people have remissions–periods when the symptoms go away–that last for months or even years. However, most patients’ symptoms eventually return. This changing pattern of the disease means one cannot always tell when a treatment has helped. Some people with ulcerative colitis may need medical care for some time, with regular doctor visits to monitor the condition.
DRUG THERAPY
The goal of therapy is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Several types of drugs are available:
Other drugs may be given to relax the patient or to relieve pain, diarrhea, or infection.
HOSPITALIZATION
Occasionally, symptoms are severe enough that the person must be hospitalized. For example, a person may have severe bleeding or severe diarrhea that causes dehydration. In such cases the doctor will try to stop diarrhea and loss of blood, fluids, and mineral salts. The patient may need a special diet, feeding through a vein, medications, or sometimes surgery.
SURGERY
About 25 percent of ulcerative colitis patients must eventually have their colons removed because of massive bleeding, severe illness, rupture of the colon, or risk of cancer. Sometimes the doctor will recommend removing the colon if medical treatment fails or if the side effects of corticosteroids or other drugs threaten the patient’s health. Surgery to remove the colon and rectum, known as proctocolectomy, is followed by one of the following:
Not every operation is appropriate for every person. Which surgery to have depends on the severity of the disease and the patient’s needs, expectations, and lifestyle. People faced with this decision should get as much information as possible by talking to their doctors, to nurses who work with colon surgery patients (enterostomal therapists), and to other colon surgery patients. Patient advocacy organizations can direct people to support groups and other information resources. (See For More Information for the names of such organizations.)
Most people with ulcerative colitis will never need to have surgery. If surgery does become necessary, however, some people find comfort in knowing that after the surgery, the colitis is cured and most people go on to live normal, active lives.
RESEARCH
Researchers are always looking for new treatments for ulcerative colitis. Therapies that are being tested for usefulness in treating the disease include:
About 5 percent of people with ulcerative colitis develop colon cancer. The risk of cancer increases with the duration and the extent of involvement of the colon. For example, if only the lower colon and rectum are involved, the risk of cancer is no higher than normal. However, if the entire colon is involved, the risk of cancer may be as much as 32 times the normal rate.
Sometimes precancerous changes occur in the cells lining the colon. These changes are called “dysplasia.” People who have dysplasia are more likely to develop cancer than those who do not. Doctors look for signs of dysplasia when doing a colonoscopy or sigmoidoscopy, and when examining tissue removed during the test.
According to the 2002 updated guidelines for colon cancer screening, people who have had IBD throughout their colon for at least 8 years and those who have had IBD in only the left colon for 12 to 15 years should have a colonoscopy with biopsies every 1 to 2 years to check for dysplasia. Such screening has not been proven to reduce the risk of colon cancer, but it may help identify cancer early should it develop. These guidelines were produced by an independent expert panel and endorsed by numerous organizations, including the American Cancer Society, the American College of Gastroenterology, the American Society of Colon and Rectal Surgeons, and the Crohn’s & Colitis Foundation of America Inc., among others.
Check Out Our Reviews & Testimonials
At Midwest GI Health we are proud to share our patient referrals from Healthgrades, Vitals, Google and Facebook. Please take some time to see how pleased our patients are with our professionalism and quality of care.
After years and years of stomach issues and having the same simple tests done with no results, I saw Dr. Taormina and he’s actually trying to help figure it all out, new tests…

The staff was very professional and friendly. The exam was explained by a nurse and the Anesthesiologist then came in to explain what she was going to do. Dr Taormina came…

The facility is small enough you don’t feel like a number and big enough you know they have what they need in case of an emergency. Dr Taormina is easy to talk to and answers all questions. Explains everything well, easy to understand. The group of nurses are also great!

Free Resources